September 26, 2016
A Look At Ibogaine
By Michael D. Shaw
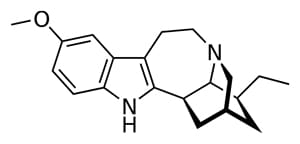
Ibogaine is a hallucinogenic drug, and one of several alkaloids found in the roots (largely), stems, and leaves of the African rain forest shrub Tabernanthe iboga. Historically, peoples of West Africa and the Congo region have used iboga extracts or chewed the root of the plant in order to remain calm but alert while stalking game. Ethnographers have also reported the use of iboga root bark during various practices of the Bwiti religion.
The plant and its properties were introduced to the West in the latter part of the 19th century. In 1901, two separate papers were published (Dybowsky & Landrin; Hailer & Heckel) in which the crystalline alkaloid was isolated, and was named “ibogaine.” Review articles on the subject note that ibogaine was marketed as a neuromuscular stimulant under the name “Lambarene” in France, from 1939-1970.
The discovery—quite by accident—of ibogaine’s anti-addictive properties is credited to New Yorker Howard Lotsof. Lotsof was a heroin user, who also experimented with other drugs, and during the early 1960s tried ibogaine, along with some of his friends. After the ibogaine ingestion, most of the group discovered that in addition to not experiencing heroin withdrawal, they no longer craved that next fix of heroin, either.
Apparently cured of addiction, Lotsof worked in the entertainment industry. At the same time, The Controlled Substances Act (Title II of the Comprehensive Drug Abuse Prevention and Control Act of 1970) was ratified by Congress, and ibogaine was included with other psychedelics as a Schedule I drug (the worst classification) with potential for abuse, and without therapeutic value.
Lotsof got re-involved with ibogaine and its value in substance abuse treatment in the 1980s, with his corporate support leading to some success in animal experiments. Not surprisingly, Big Pharma would show little interest, given the drug’s history, and the fact that ibogaine is naturally-occurring. The difficulties in getting approval to work with Schedule I substances did not help either.
Nonetheless, promising results appeared in Dutch clinical trials, and in work done at the University of Miami in the early 1990s. However, funding issues and the death in 1993 of a Dutch patient—although not conclusively attributed to ibogaine—forced this work into other settings. Such other settings were dubbed the “ibogaine medical subculture,” in an eponymous 2008 article in Journal of Ethnopharmacology, co-authored by Lotsof.
This landmark study examined only treatment providers who had already publicly identified their activities by maintaining websites; publishing in the lay or scientific press; presenting at public meetings; or posting to ibogaine list servers. Among the findings:
- An estimated 3,414 individuals had taken ibogaine as of February 2006, with 68% of the total having taken it for the treatment of a substance-related disorder, and 53% specifically for opioid withdrawal.
- The existence and expansion of the subculture indicates a demand for new treatment, which is sought regardless of medical risk, inconvenience, expense, and in some cases legal prohibition.
- Ibogaine’s effect in opioid withdrawal is consistent with case studies and preclinical evidence, and is unlikely to be mediated by placebo.
A bravura 11,600-word review article (2013)—by UC San Diego anthropologist Thomas Kingsley Brown—entitled “Ibogaine In The Treatment of Substance Dependence” cites a host of animal studies that demonstrate ibogaine’s efficacy. Even more impressive are the studies he cites in humans, most of which did involve small groups. Copious details are provided in the review, along with 109 references.
We can draw some key points from the article’s “Discussion” section…
- The human studies of ibogaine treatment provide some preliminary support for the efficacy of ibogaine in alleviating the considerable discomforts of withdrawal from opiates and other addictive drugs, and thereby in facilitating detoxification from these substances in a comparatively painless manner.
- The limited research results achieved so far suggest that opiate and cocaine cravings are significantly reduced for up to one month following treatment and that a substantial minority of patients remain abstinent for several months.
Of course, much more research on ibogaine needs to be done. And, that means reducing the onerous restrictions inherent in Schedule I substances.
