- peroxide is used as a liquid or vapor for disinfection, sterilization, and decontamination by healthcare professionals.
- Hydrogen peroxide is a hazard and can affect the eyes, skin, and respiratory system. As it is a strong oxidizer, it can react with organic compounds.
- Continuous point-of-care detection is necessary to determine the measures personnel need to protect themselves against hydrogen peroxide hazards.
Hydrogen peroxide is commonly used in the healthcare industry for disinfection, sterilization, and decontamination. However, this ubiquitous compound can be a hazard, and people in the industry should be aware of the risks involved and mitigation methods. Detecting hydrogen peroxide accurately is one of the most crucial steps to prevent hazards.
Detecting Hydrogen Peroxide in Healthcare
Hydrogen peroxide (H2O2) is a colorless, noncombustible liquid that is a crystalline solid below 12°F (-11.1°C). It is liquid in 3% to 6% dilutions in healthcare facilities. The chemical is also a vapor from 30-35% liquid H2O2.
Hydrogen peroxide is used in the healthcare industry for disinfection and sterilization, as it has bactericidal, virucidal, fungicidal, and sporicidal properties. The compound produces no toxic waste; its products are water vapor and oxygen.
It is used for materials and devices which cannot be sterilized using high temperatures and humidity, like electrical medical devices, some plastics, and metal alloys susceptible to corrosion. H2O2 is suitable for sterilizing over 95% of medical devices.
Some of the concentrations in which liquid hydrogen peroxide is used in the healthcare industry for disinfection are as follows:
- 3% hydrogen peroxide is used on inanimate surfaces.
- 3% to 6% H2O2 is suitable for soft contact lenses, ventilators, tonometer biprisms, and endoscopes. It is also effective in spot-disinfecting fabrics.
Hydrogen peroxide vapor is also suitable for sterilization in new low-temperature “no-touch” systems and has broad applications to control healthcare-associated pathogens.
- It is used to sterilize reusable metal and nonmetal instruments and materials.
- The vapor is used to decontaminate rooms and furniture in healthcare institutions. Vaporized hydrogen peroxide was effective against SARS-CoV-2 and was used during the COVID-19 pandemic to decontaminate medical and pharmaceutical manufacturing facilities, business offices, classrooms, and confined spaces.
However, the vapor system is unsuitable for liquids, powders, linens, and cellulose materials.
Hydrogen peroxide has the advantage that it doesn’t need to be activated before use. However, its hazards must also be kept in mind.
Hydrogen Peroxide Hazards
Hydrogen peroxide is unstable and decomposes into oxygen and water at ordinary temperatures.
The oxygen it produces makes it a strong oxidizing agent that causes spontaneous combustion in contact with organic materials leading to fires and explosions. Liquid H2O2 also attacks some plastics, rubber, and coatings, causing them to ignite.
The rate of H2O2 decomposition doubles for every 10°C rise in temperature. It can decompose faster than container vents let out, leading to pressure buildup. Higher temperatures or concentrations over 90% will lead to detonation. H2O2 also decomposes when exposed to light.
Hydrogen peroxide reacts with catalytic metals such as iron, brass, copper, bronze, lead, zinc, chromium, silver, and manganese and their compounds, producing oxygen and heat, which will also increase container pressure. This reaction with metals can also be an operational issue in using these metals as containers for H2O2.
Hydrogen peroxide causes systemic toxicity on inhalation and ingestion but is not absorbed through the skin. It can be consumed accidentally, or unrinsed hydrogen peroxide-soaked tonometer tips can harm people.
Health Effects
Hydrogen peroxide affects the skin, eyes, and respiratory system. As the concentration of H2O2 increases, symptoms become more severe.
Acute Exposures
Acute exposure to H2O2 gas can irritate the eyes, skin, and throat. Hydrogen peroxide >10% concentrations can be corrosive to these organs.
Gastrointestinal: Accidental ingestion can cause sudden formation of oxygen. Ingestion of 3-10% H2O2 produces mild irritation, gastric distension, internal bleeding, and embolism.
Respiratory: Hydrogen peroxide vapors or aerosols cause upper airway irritation, nose inflammation, shortness of breath, and burning or tightness in the chest. Higher levels of 10-20% H2O2 gas cause congestion and delayed accumulation of fluids in the lungs, inducing unconsciousness and then respiratory arrest. Severe inhalation causes permanent lung damage. Children are more vulnerable as their airways have smaller diameters.
CNS: High concentrations also cause seizures, cerebral infarction or embolism, permanent neurological deficits, and death.
Eyes: H2O2 solutions cause stinging pain or tearing of the eyes; concentrations >5% can cause eye injury. Corneal damage can occur due to H2O2-contaminated tonometer tips. Severe cases lead to blindness.
Skin: Repeated exposures to vapor cause temporary bleaching of hair and skin. Liquid H2O2 causes skin burns.
Chronic Effects
Hydrogen peroxide decomposes rapidly in the body, and the chances of chronic toxicity are low. However, people exposed repeatedly to hydrogen peroxide vapor could suffer chronic respiratory tract irritation and lung collapse. Repeated contact with H2O2 vapor or solution can bleach skin and hair. Children will suffer more because of longer latency periods.
Exposure Limits
In the US, the National Institute for Occupational Safety and Health (NIOSH) and Occupational Safety and Health Administration (OSHA) have set the following exposure limits in parts per million (ppm):
OSHA PEL (permissible exposure limit),
total weight average (TWA) averaged over an 8-hour work shift : 1 ppm (1.4 mg/m3)
NIOSH Recommended exposure limit (REL) TWA : 1 ppm (1.4 mg/m3)
NIOSH IDLH (immediately dangerous to life or health) : 5 ppm
AIHA ERPG-2 (emergency response planning guideline) : 50 ppm
(Maximum airborne concentration for exposure up to 1 hour
without causing irreversible or serious health effects or impair
an individual’s ability to take protective action.)
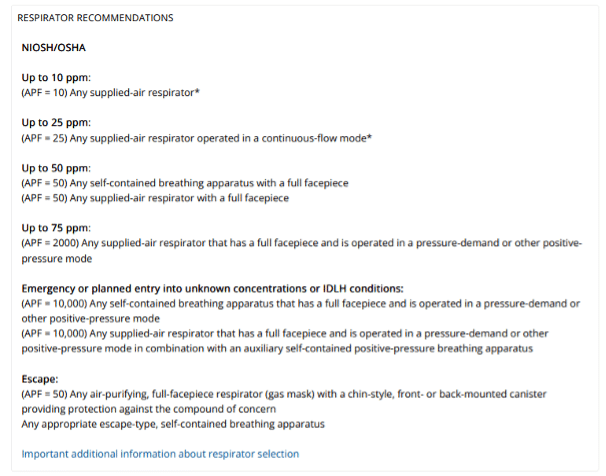
Measures to Prevent H2O2-Related Injuries
Knowing the acute and chronic effects hydrogen peroxide can have, healthcare professionals should take steps to avoid exposure. Some NIOSH recommendations are discussed below but are not an exhaustive list. Visit NIOSH’s website on “Managing Chemical Safety in the Workplace,” to learn more about controlling workplace exposures.
- Read the chemical labels and accompanying safety data sheets for information on H2O2 hazards.
- Take special precautions during storage, keep H2O2 below 25°C, and protect from light to prevent compound decomposition. Store H2O2 in amber-colored glass bottles to protect the chemical against light.
- Monitor the dilution of H2O2 by testing regularly to ensure the concentrations.
- Use proper protective clothing to ensure that personnel working with H2O2 during the sterilization, infection, or decontamination do not come in contact with liquid or gas H2O2. Table 1 provides the NIOSH recommendations for protective clothing for dealing with H2O2 of different concentrations.
- In case of contact with H2O2, wash the skin with water. Eyewash is necessary for a quick drench. Remove clothing that is wet or contaminated.
Table 1: Protective wear recommended by NOISH when using H2O2 of varying concentrations. (Credit: https://www.cdc.gov/niosh/npg/npgd0335.html#print)
Testing and detecting hydrogen peroxide levels are essential for the preventive measures to be effective. Therefore, accurate and timely detection should also be part of the safety measures.
Detecting Hydrogen Peroxide
To decide which protective gear personnel must use, they need to know the H2O2 levels they are dealing with. Monitoring treated areas to ensure the H2O2 levels are below specified thresholds is also necessary. Therefore continuous monitoring and point-of-care detection are necessary. Healthcare professionals can use sensor-based detectors for both of these purposes.
Using sensor-based detectors is a viable option since they are portable, give readings in real-time, are cost-effective, and are easy to use by nonspecialized technicians. Since H2O2 is very reactive, its detection is based on the reaction of molecules with a sensor’s surface. Of the two colorimetric and electrochemical methods, the latter is favored because it is more sensitive, has a shorter response time, and miniaturization.
The usual factors of detection range, detection limit, sensitivity, selectivity, and stability, apply while choosing a detector. H2O2 detectors for healthcare professionals must also have a low detection level and high performance.
In the healthcare environment, some additional points must also be considered. These are biocompatibility, toxicity, and low sample volume necessary for analysis. When detecting hydrogen peroxide, the device must also be mechanically flexible.
The Interscan Hydrogen Peroxide Detector
Interscan’s GasD® 8000 portable gas analyzers offer five options for H2O2 detection. All of them are portable, come with visual and audio alarms, and have data logging possibilities. It is possible to choose Interscan detectors with varying sensitivity and detection range as specified below:
GasD 8000 Series Portable Gas Analyzers – Hydrogen Peroxide:
8090-1000m has a detection range of 0-1000 ppm and a resolution of 1 ppm.
8090-20.00m measures 0-20 ppm with a resolution of 0.01 ppm.
8090-200.0m has a detection range of 0-200 ppm and resolution of 0.1 ppm.
8090-2000b that can measure ranges as low as 0-2000 parts per billion (ppb) with a resolution of 1 ppb.
8090-5.00m has a detection range of 0-5 ppm and resolution of 0.01 ppm.
8090-50.0m measures a range of 0-50 ppm with a resolution of 0.1 ppm.
Just as it is vital to sterilize healthcare facilities to safeguard patients’ health, it is also necessary to monitor the environment for hydrogen peroxide to ensure it doesn’t harm professionals using it.
Written By:

Vijayalaxmi Kinhal
Science Writer, CID Bio-Science
Ph.D. Ecology and Environmental Science, B.Sc Agriculture
Sources
ATSDR. (2014, October 21). Medical Management Guidelines for Hydrogen Peroxide. Retrieved from https://wwwn.cdc.gov/TSP/MMG/MMGDetails.aspx?mmgid=304&toxid=55
CDC. (1978). Occupational Health Guideline for Hydrogen Peroxide. Retrieved from https://www.cdc.gov/niosh/docs/81-123/pdfs/0335.pdf
CDC. (2016, September 18). Chemical Disinfectants- Guideline for Disinfection and Sterilization in Healthcare Facilities. Retrieved from https://www.cdc.gov/infectioncontrol/guidelines/disinfection/disinfection-methods/chemical.html#Hydrogen
Giaretta, J. E., Duan, H., Oveissi, F., Farajikhah, S., Dehghani, F., & Naficy, S. (2022). Flexible sensors for hydrogen peroxide detection: A critical review. ACS Applied Materials & Interfaces, 14(18), 20491–20505. https://doi.org/10.1021/acsami.1c24727
Hydrogen Peroxide Solution 6% BP 20 Vols. (2022, July 8). Retrieved from https://www.medicines.org.uk/emc/product/4869/smpc/print
National Institute for Occupational Safety and Health. (2019, June 21). Hydrogen Peroxide. Retrieved from https://www.cdc.gov/niosh/topics/hydrogen-peroxide/default.html
National Institute for Occupational Safety and Health. (2019, October 30). Hydrogen peroxide. Retrieved from https://www.cdc.gov/niosh/npg/npgd0335.html
Rutala, W. A., & Weber, D. J. (2015). Disinfection, sterilization, and control of hospital waste. In Mandell, Douglas, and Bennett (Eds.), Principles and Practice of Infectious Diseases ( Eight Edition). https://doi.org/10.1016/b978-1-4557-4801-3.00301-5